Recognizing the Whisper Before the Shout
Why subtle signs of withdrawal matter more than dramatic detox scenes
Hollywood often glamorizes detox with violent shakes, dramatic vomiting, and hospital sirens. Real life usually starts quieter, with early warning signs of withdrawal that whisper before they roar. A person may shrug off mild muscle aches after the last dose, believing it is normal tension. They might ignore a brief surge of sweating and chills during detox, claiming the room feels warm. These subtle signs of withdrawal signal the body’s first struggle to regain balance and deserve immediate attention.
Overlooking these common withdrawal symptoms to watch can delay safe medical supervision, turning a manageable phase into a crisis. Minor digestive upset or a slightly rapid heart rate in withdrawal can evolve into serious dehydration or cardiac strain. Early recognition allows time to prepare hydration strategies and adjust nutrition for withdrawal recovery. It also helps loved ones coordinate a support group near you, reducing isolation right from the start.
How physical dependence indicators set the stage for recovery choices
Physical dependence develops when opioid receptors or other neural pathways adapt to chronic drug use. The body adjusts its chemistry, so stopping suddenly shocks every system. Tight calves, restless legs in opiate withdrawal, or gentle tremors are not random annoyances; they mark neurochemical shifts. Such indicators help clinicians gauge the safest tapering plan with a clinician and select medications that ease muscle aches.
Spotting these physical dependence indicators early also guides practical decisions about care locations. Someone experiencing psychological symptoms of withdrawal, like rising anxiety, may benefit from inpatient observation rather than outpatient visits. Recognizing temperature fluctuations during withdrawal can prompt monitoring equipment to prevent dangerous spikes. Each small clue informs when to seek medical supervision, shaping treatment paths long before severe withdrawal symptoms appear.
The risk of relapse when early clues go unnoticed
Ignoring the body’s first murmurs often fuels the risk of relapse. Cravings and risk of relapse increase when discomfort grows unchecked, pushing a person to seek fast relief from addictive substances. Depression in early recovery can deepen if rapid mood swings surprise both individual and family member observers. Anxiety snowballs into panic attacks during early abstinence, leading many to abandon progress.
A timely response to these early whispers supports momentum toward lasting change. Engaging a support group guidance for withdrawal supplies accountability and emotional grounding during vulnerable hours. Clinicians can introduce mindfulness techniques for cravings before they spiral. Families trained to notice subtle behavior shifts can encourage hydration during detox recovery and advocate for professional help. Small, early actions often decide whether acute discomfort evolves into renewed drug dependence or into steady, hopeful healing.
Reading the Body’s First Murmurs of Withdrawal
Muscle aches after the last dose and the role of opioid receptor hyperactivity
Many people notice dull muscle aches after the last dose of prescription medications yet dismiss them as routine strain. Such discomfort often signals opioid receptor hyperactivity, a common early sign of withdrawal that develops when receptors suddenly lose their usual stimulation. The central nervous system responds by firing erratic pain signals through the body, intensifying soreness in the back, shoulders, and calves. Understanding this mechanism helps explain why light stretching rarely eases these aches; the cause is chemical, not purely physical. Recognizing the neurobiological root encourages individuals to seek medical supervision rather than pushing through pain alone.
The presence of muscle aches does more than announce physical dependence; it shapes safe tapering decisions. Clinicians often use non-opioid analgesics or acupuncture to soothe receptor rebound without reinforcing drug addiction. Identifying pain location and intensity also aids timing in the withdrawal process, revealing whether receptors are stabilizing or still spiking. Early acknowledgement prevents unnecessary suffering, lowers risk of relapse, and strengthens commitment to healthy coping strategies. When muscle soreness pairs with fatigue, hydration and gentle movement become vital companions in any safe withdrawal plan.
Sweating and chills during detox as temperature fluctuation red flags
Sudden sweating and chills during detox represent more than discomfort; they mark competing surges of adrenaline and serotonin as the body recalibrates. These temperature swings can occur with any type of drug yet appear prominently in alcohol withdrawal symptoms and opiate withdrawal cases. Although many people blame a warm room or cool breeze, alternating damp shirts and goosebumps reveal autonomic distress demanding attention. Monitoring body temperature helps differentiate a common withdrawal symptom from infection or other medical emergencies. Documenting patterns also enables providers to adjust taper schedules or prescribe supportive medications.
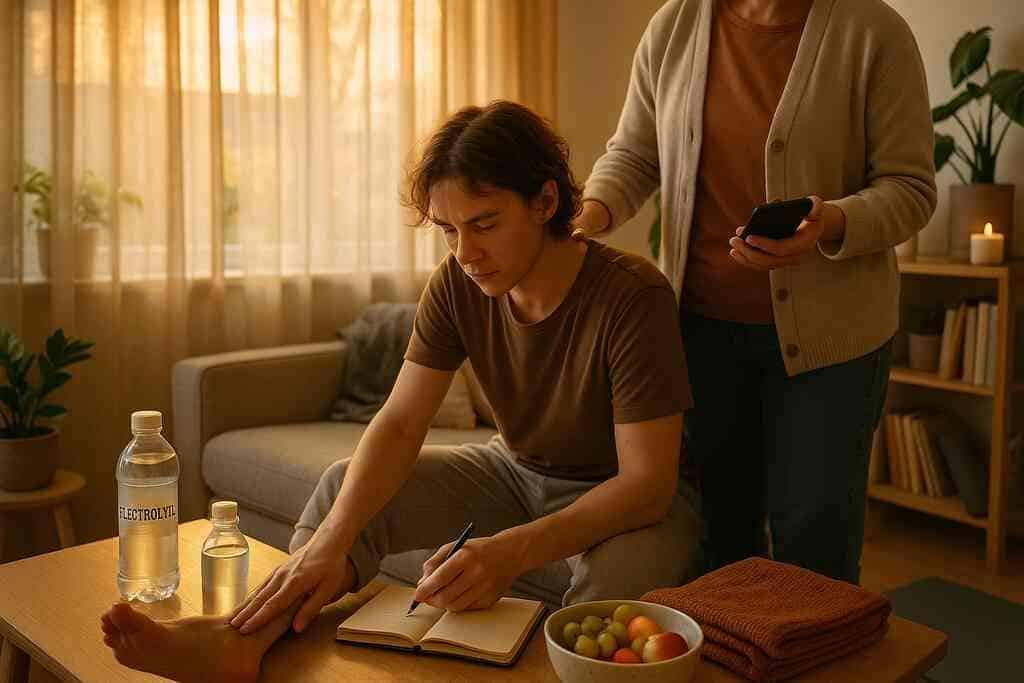
Ignoring these red flags may amplify dehydration, cramping, and dizziness, complicating the withdrawal timeline. Regular fluid intake with electrolytes mitigates sweat-related losses, while layered clothing eases sudden chills. Breathing exercises calm the sympathetic nervous system, reducing adrenaline spikes that trigger sweating episodes. Family member support can help track clothing changes and fluid counts, offering objective data when cravings cloud judgment. Small adjustments provide powerful reassurance that the body’s thermostat will eventually reset with consistent care.
Rapid heart rate nausea and digestive upset across drug types
A racing pulse often joins nausea during opioid taper or stimulant cessation, reflecting overstimulated cardiac receptors and disrupted gut motility. Each heartbeat may feel exaggerated, echoing anxiety while amplifying psychological symptoms of withdrawal. Coupled with digestive upset, this duo can frighten those unprepared for its intensity, sending many back to addictive substances for quick relief. Recognizing it as a predictable sign of withdrawal prevents unnecessary panic and promotes proactive management.
Slow, diaphragmatic breathing lowers heart rate, and ginger tea or bland foods soothe unsettled stomachs without conflicting with medications. Clinicians may recommend beta-blockers or antiemetics under medical care to stabilize these systems. Tracking pulse and nausea frequency helps map individual drug withdrawal timeline awareness, guiding hydration, nutrition, and rest schedules. Addressing cardiac and gastrointestinal discomfort early reduces relapse risk and restores confidence in the body’s capacity to heal.
Restless legs tremors and insomnia that follow opioid tapering
Restless legs in opiate withdrawal often strike at night, producing crawling sensations that sabotage sleep and fuel exhaustion. Tremors may accompany these movements, reflecting nerve repolarization as opioid receptor hyperactivity declines. Without rest, the brain struggles to regulate mood, increasing depression in early recovery and intensifying cravings. Many mistake sleeplessness for personal weakness rather than a physiological symptom of drug dependence. Framing insomnia as a phase promotes patience and practical solutions.
Warm baths, magnesium supplements, and mindfulness techniques for cravings can relax jittery limbs and quiet the racing mind. Timed release melatonin or non-addictive sleep aids may be introduced with clinician oversight when self-care fails. Establishing regular bedtime rituals signals the nervous system to slow, aligning circadian rhythms disrupted by former drug use. Each restful night empowers the next day’s recovery efforts, transforming a subtle sign of withdrawal into evidence of progress.
Spotting drug withdrawal timeline patterns to time medical care
Every substance presents unique onset and peak periods for symptoms of drug withdrawal, yet patterns emerge when observed closely. Opioids often produce muscle aches and yawning within twelve hours, while alcohol may unleash tremors and anxiety slightly later. Stimulant withdrawal can delay fatigue until a full day passes, then plunge energy levels suddenly. Mapping these sequences helps determine when to seek medical supervision versus when home support suffices. Timely intervention curbs severe withdrawal symptoms before they escalate into seizures, delirium, or cardiac events.
Keeping a daily log of physical dependence indicators, from sweating episodes to rapid heart rate, creates a personalized timeline. This record allows health professionals to adjust taper dosing and anticipate psychological symptoms such as irritability or hallucinations. It also guides families in scheduling check-ins, meals, and hydration reminders during high-risk hours. By understanding typical timelines, individuals align expectations with reality, lowering anxiety and bolstering resilience. Signs of Withdrawal offers educational resources that support this tracking process, empowering people to navigate each milestone with informed confidence.
Unmasking the Mind’s Subtle Cries
The brain often whispers long before it screams, and those faint cognitive murmurs can steer the entire withdrawal process. Emotional turbulence may seem less dramatic than shaking hands, yet psychological symptoms of withdrawal erode resolve quickly. Because mental health shifts can appear and vanish within hours, many people mislabel them as ordinary mood swings. Recognizing these early warning signs of withdrawal lets individuals secure medical supervision and prevent sudden relapse. With clarity, families and clinicians can transform invisible dangers into structured recovery actions.
Alcohol withdrawal anxiety panic attacks and racing thoughts
Anxiety in alcohol withdrawal rarely begins with a bang; instead, it unfurls as a constant edge that colors every thought. The individual may wake trembling, convinced that routine noises signal catastrophe, even before severe withdrawal symptoms appear. Racing thoughts then loop relentlessly, amplifying each physical sensation until panic attacks erupt. Such episodes increase heart rate, compromise sleep, and spike cortisol, weakening immunity during an already taxing detox phase. Early acknowledgment turns this subtle sign of withdrawal into a cue for calm breathing exercises and, when needed, short-term anxiolytics under medical care.
Ignoring alcohol withdrawal anxiety heightens the risk of relapse because the mind aggressively seeks relief from fear. People tempted to go cold turkey often underestimate how quickly terror overtakes willpower. Timely reassurance from a support group near you reduces isolation, while guided meditation steadies spiraling cognition. Clinicians may suggest gradual tapering rather than abrupt cessation to soften neurochemical shocks driving panic. Consistent monitoring of thought speed and intensity offers measurable proof that progress is happening, even when anxiety still whispers.
Cravings depression and post acute withdrawal syndrome clues
Cravings rarely shout; they manifest as a gentle mental tug, promising comfort if the last dose returns. When paired with depression in early recovery, that tug becomes magnetic, pulling attention toward memories of drug use. Feelings of emptiness, guilt, or apathy signal dopamine pathways aching for stimulation and mark the onset of post acute withdrawal syndrome, also called PAWS. Recognizing that dull heaviness as a symptom-not personal failure-protects self-esteem and supports treatment adherence. Structured routines, balanced nutrition, and mindful movement can replenish neurochemical reserves without addictive substances.
During this stage, subtle shifts often precede relapse. A once-chatty friend grows silent, or hobbies lose spark, yet these indicators may go unnoticed by the recovering person. Family member observation becomes critical, offering external insight when self-awareness falters. Documenting mood scores daily helps spot patterns, allowing clinicians to adjust therapy or medication before despair deepens. Consistency anchors fragile motivation, turning cravings and depression into signposts that guide further intervention rather than derailment.
Hallucinations nightmares and psychological symptoms that demand supervision
Visual or auditory distortions sometimes surface quietly, beginning with fleeting shadows at the edge of vision. Nightmares then invade sleep, replaying traumatic moments or inventing frightening scenes, leaving the individual exhausted by dawn. Although these phenomena often occur during severe alcohol detox or advanced opiate withdrawal, they sometimes start earlier as mild sensory shifts. Because hallucinations can escalate to dangerous confusion, immediate medical supervision is essential. Rapid evaluation distinguishes withdrawal-related psychosis from primary psychiatric disorders and drives appropriate medication choices.
Nighttime terrors also worsen insomnia, compounding cognitive fatigue and raising the risk of relapse. Consistent bedtime rituals, light exposure earlier in the day, and precise hydration strategies can temper nightmare frequency. If vivid dreams persist, clinicians might prescribe non-addictive sleep aids while monitoring respiratory health. Through proactive management, frightening images gradually lose dominance, and restful sleep becomes realistic again. Each reclaimed night represents a milestone toward stable mental health.
Family member observations of mood swings and behavioral changes
Loved ones often notice subtle behavioral changes before the recovering person does. A sudden withdrawal from conversation, abrupt irritability at minor frustrations, or unexplained laughter can reveal neurotransmitter volatility. Because shame often silences self-reporting, family observations supply crucial data for clinicians mapping drug withdrawal timeline awareness. Clear, compassionate communication converts what could feel like surveillance into collaborative care. When patterns emerge, professional support can adjust tapering schedules or introduce therapy sessions promptly.
However, families must balance vigilance with respect, avoiding accusations that ignite defensiveness. Using objective language-describing specific actions rather than labeling personality-maintains trust. Support group guidance for withdrawal teaches relatives how to record events and share them constructively with treatment teams. Such documentation prevents misinterpretation of symptoms as deliberate misconduct, keeping focus on healing. Ultimately, engaged families create a recovery environment where early warning signs appear and are addressed long before crisis unfolds, a principle championed by Signs of Withdrawal as it connects households with evidence-based resources.
Navigating the Critical Juncture From Signals to Solutions

Early warning signs offer a narrow window where decisive action prevents chaos. Navigating that juncture demands practical knowledge, timely support, and unflinching honesty about substance abuse risks. By converting subtle alerts into structured plans, individuals replace panic with purposeful motion toward recovery. This section explores key strategies that shift attention from frightening symptoms to concrete, evidence-based solutions. Each subsection delivers actionable guidance, empowering readers to bridge the gap between recognition and sustainable healing.
Cold turkey dangers versus a safe tapering plan with a clinician
Dropping addictive substances abruptly, often called going cold turkey, can seem courageous yet carries significant physiological perils. When opioid receptors lose stimulation overnight, blood pressure spikes, seizures threaten, and severe withdrawal symptoms intensify without warning. Psychological symptoms of withdrawal, including paranoia and depression, likewise accelerate, overwhelming even determined individuals. Family members may misinterpret these crises as stubbornness rather than neurochemical distress, delaying emergency medical care. Recognizing cold turkey dangers encourages a proactive conversation with qualified clinicians before discontinuing any type of drug.
A safe tapering plan gradually reduces dosage, permitting receptor systems to recalibrate while maintaining relative stability. Clinicians monitor muscle aches, trembling, and temperature fluctuations during withdrawal, adjusting schedules to prevent dangerous rebounds. Structured tapering also lowers risk of relapse because discomfort remains tolerable, reinforcing self-efficacy each day. In many cases, adjunct medications ease nausea during opioid taper and calm rapid heart rate in withdrawal. Documented protocols further allow insurance approval for withdrawal treatment in outpatient or inpatient settings, protecting continuity of care.
Hydration nutrition and mindfulness techniques for cravings control
Cravings surge when dehydration meets blood sugar instability, making simple physiological fixes powerful relapse deterrents. Frequent sips of electrolyte water replace minerals lost through sweating and chills during detox, sustaining cardiac balance. Balanced meals containing complex carbohydrates smooth glucose curves, preventing sudden fatigue that the brain mislabels as drug hunger. Integrating lean protein supports neurotransmitter synthesis, fostering mood steadiness through early recovery. Planning snacks ahead removes decision fatigue, a subtle trigger for impulsive drug use.
Mindfulness techniques complement biologic strategies by interrupting automatic reach-for-relief habits. Slow diaphragmatic breathing reduces rapid heart rate, while body scans spotlight transient muscle tension instead of catastrophic thinking. Visualizing cravings as passing waves reframes them, granting confidence that no sensation lasts forever. Regular meditation sessions also strengthen prefrontal circuits weakened by chronic drug abuse, improving impulse control. Together, hydration, nutrition, and mindfulness form a three-part shield guarding progress during the withdrawal process.
Leveraging a support group near you to counter isolation
Isolation magnifies anxiety and distorts perception, especially when insomnia and restless legs in opiate withdrawal disrupt nights. A support group near you provides immediate empathy, shared strategies, and practical accountability against secretive drug use. Hearing peers describe identical sweating episodes or nausea validates experience and neutralizes shame. Groups also teach families to observe mood swings without judgment, shifting household dynamics toward compassionate vigilance. Consistent attendance correlates with lower relapse rates because community reinforces each milestone, however small.
Choose meetings that match your substance use disorder profile, whether alcohol, stimulants, or prescription drugs. Virtual formats expand reach for rural residents seeking withdrawal treatment near limited medical infrastructure. Rotating leadership prevents dominance by any member, ensuring fresh perspectives and balanced guidance. Many support circles maintain directories of addiction treatment centers near meeting locations for seamless referrals. Therefore, group involvement becomes both a social anchor and a gateway to higher levels of care if necessary.
Mapping addiction treatment centers in the state of choice for continuum care
Recovery rarely follows a straight line; instead, needs evolve from detox to therapy to long-term maintenance. Mapping addiction treatment centers in the state of residence establishes clear pathways before emergencies arise. Start with accredited facilities offering medical supervision for severe drug withdrawal symptoms, including hallucinations or cardiac instability. Next, identify outpatient programs emphasizing cognitive behavioral therapy, vocational support, and relapse-prevention skills. Finally, explore sober living environments that extend structure once intensive services conclude.
Geographic planning matters because transportation hurdles derail appointments and strain motivation. Search phrases like withdrawal treatment near me or addiction treatment centers in the state of create practical lists quickly. Compare services, insurance acceptance, and specialty tracks for co-occurring mental health disorders. Maintain contacts for at least two backup facilities in case waitlists appear unexpectedly. This strategic map transforms an overwhelming system into an organized menu of options, reducing crisis-time chaos.
Using Signs of Withdrawal resources to connect with medical supervision quickly
Even comprehensive maps cannot cover every variable, which is why an adaptive directory accelerates decision making. Signs of Withdrawal synthesizes verified data on addiction treatment centers near diverse communities, updating entries continually. Users filter by substance, insurance, and desired intensity, revealing withdrawal treatment in minutes rather than days. The platform also highlights facilities experienced with post acute withdrawal syndrome, a frequent relapse culprit. Access to such targeted information empowers families to secure medical care before subtle sign of withdrawal escalates.
Beyond listings, the resource library explains cold turkey dangers, safe tapering plans, and nutrition for withdrawal recovery. Printable worksheets guide symptom tracking, assisting clinicians who rely on accurate timelines for medication adjustments. Interactive support forums connect users with peers navigating similar stages, diminishing isolation between appointments. Because the directory spans all fifty states, relocation or travel no longer interrupts continuity of treatment. Ultimately, streamlined access to expertise converts early warning signs into decisive, life-affirming action steps.
Transforming Warning Signs Into Recovery Catalysts
Turning early withdrawal alerts into actionable treatment steps
Recognizing a subtle sign of withdrawal becomes powerful only when converted into concrete action. First, document every muscle ache after the last dose in a daily journal. Then share these specific symptoms of withdrawal with medical supervision to shape a safe tapering plan. Because physical dependence indicators fluctuate, update notes when sweating and chills during detox appear. This simple record transforms vague discomfort into objective data that guides timely treatment decisions.
First, acknowledge cold turkey dangers that jeopardize stability. Next, align the journal with clear milestones. Schedule hydration checkpoints to counter rapid heart rate in withdrawal and prevent dizziness. Prepare balanced snacks that stabilize blood sugar, reducing cravings and risk of relapse. If restless legs in opiate withdrawal disturb sleep, plan mindfulness techniques before bedtime rather than reactive panic. Finally, keep contact information for addiction treatment centers near preferred locations, ensuring immediate escalation if severe withdrawal symptoms emerge.
Sustaining long term mental health beyond the acute detox window
Acute detox often fades within days, yet psychological symptoms of withdrawal can linger for months. Post acute withdrawal syndrome may trigger depression waves in early recovery, challenging drug withdrawal timeline awareness. Therefore, establish routine mental health check-ins just as diligently as physical assessments. Use mood rating scales alongside craving logs to reveal subtle trends before they escalate. Early detection lets clinicians adjust therapy or non addictive medication, maintaining stability during vulnerable transitions.
Structured self-care sustains progress between appointments. Regular exercise boosts dopamine pathways bruised by prolonged drug use, lifting motivation naturally. Consistent sleep hygiene counters insomnia after stopping drugs, protecting cognition and judgment. Balanced social activities replace isolation, providing immediate feedback if irritability or avoidance resurfaces. Together, these habits form a proactive shield that preserves mental health long after the last physical cramp has passed.
Embracing hope resilience and community on the recovery journey
Hope begins as a fragile whisper yet grows louder when reinforced by shared stories of survival. Support group guidance for withdrawal offers immediate evidence that change is possible, even after years of substance abuse. Hearing peers discuss muscle aches, nausea, and eventual relief reframes suffering as temporary rather than defining. Moreover, witnessing others navigate setbacks teaches resilience, a critical quality when cravings strike unexpectedly. Each meeting transforms isolation into collective courage.
Cultivating gratitude further anchors optimism. Daily reflection on small victories, like reduced trembling or steady pulse, counterbalances memories of drug dependence. Writing these observations reinforces neural pathways that favor perseverance over avoidance. When gratitude pairs with realistic goal setting, setbacks shrink and momentum accelerates. Consequently, the recovery journey evolves from a series of fearful milestones into an inspiring narrative still unfolding.

