An ostomy is a life-changing medical procedure that affects millions of people worldwide, yet it is still widely misunderstood. Many patients and caregivers search for answers to questions like what causes ostomy, how it impacts daily life, and whether it is permanent or temporary. While the idea of an ostomy can feel overwhelming at first, modern medical advances, improved ostomy care products, and better education have made it possible for people with ostomies to live full, active, and independent lives.
This article provides a clear, comprehensive overview of ostomy surgery—why it is performed, the different types of ostomies, and what life looks like after the procedure. Whether you are preparing for surgery, supporting a loved one, or simply seeking reliable information, understanding the basics can significantly reduce fear and uncertainty.
What Is an Ostomy?
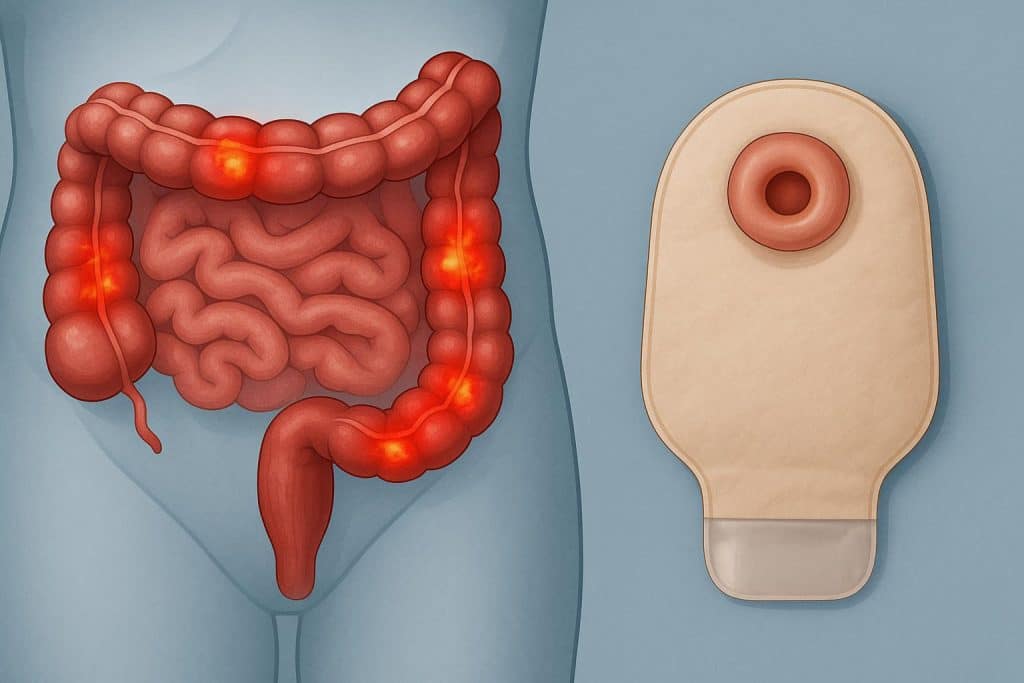
An ostomy is a surgically created opening (called a stoma) that allows bodily waste to exit the body when the normal digestive or urinary pathways are not functioning properly. The stoma is usually formed on the abdomen, where waste is collected in a specialized external pouching system.
Unlike many surgical procedures, an ostomy does not define a disease—it is a solution. Ostomies can be temporary or permanent, depending on the underlying medical condition and the patient’s recovery potential.
What Causes Ostomy?
Understanding what causes ostomy requires looking at the medical conditions that damage or bypass parts of the digestive or urinary system. Doctors recommend ostomy surgery only when it is medically necessary and often life-saving.
1. Inflammatory Bowel Diseases (IBD)
Chronic inflammatory conditions are among the most common reasons for ostomy creation.
- Crohn’s disease can cause deep inflammation, strictures, and fistulas anywhere in the digestive tract.
- Ulcerative colitis primarily affects the colon and rectum, sometimes leading to severe complications that require removal of the colon.
When inflammation becomes unmanageable or dangerous, an ostomy may be required to allow the bowel to heal or to replace its function entirely.
2. Colorectal and Bladder Cancer
Cancer is another leading cause of ostomy surgery.
- Colorectal cancer may require partial or total removal of the colon or rectum.
- Bladder cancer can necessitate urinary diversion if the bladder must be removed.
In these cases, an ostomy allows waste elimination after affected organs are surgically removed to prevent cancer spread.
3. Traumatic Injury or Emergency Surgery
Severe trauma to the abdomen—caused by accidents, violence, or emergency complications—can damage intestines or urinary organs beyond immediate repair. An ostomy may be created as a temporary or permanent measure to stabilize the patient and preserve life.
4. Congenital Conditions
Some individuals are born with digestive or urinary system abnormalities, such as:
- Imperforate anus
- Hirschsprung’s disease
- Spina bifida
In these situations, ostomy surgery may be necessary early in life to ensure proper waste elimination.
5. Severe Infections and Bowel Obstruction
Conditions such as diverticulitis, bowel ischemia, or perforation can cause life-threatening infections. When the bowel cannot safely function, creating an ostomy reduces pressure, prevents leakage, and allows healing.
Types of Ostomies
The type of ostomy depends on which organ is involved and what function needs to be bypassed or replaced.
Colostomy
A colostomy connects part of the colon to the abdominal wall. Stool consistency varies depending on the location of the stoma in the colon and may range from solid to semi-formed.
Colostomies can be temporary or permanent and are often associated with colorectal cancer or diverticular disease.
Ileostomy
An ileostomy is created using the ileum (the final part of the small intestine). Output is usually liquid to semi-liquid and contains digestive enzymes, making proper skin protection essential.
Ileostomies are common in patients with inflammatory bowel disease.
Urostomy
A urostomy diverts urine away from the bladder using a section of the intestine to create a channel. Urine continuously drains into an external pouch.
Urostomies are often required after bladder removal due to cancer or severe dysfunction.
Temporary vs. Permanent Ostomy
Not all ostomies last a lifetime.
- Temporary ostomies are created to allow healing after surgery or trauma. Once the affected organ recovers, a reversal surgery may be possible.
- Permanent ostomies are necessary when organs are removed or permanently damaged.
Your healthcare team determines the type based on medical necessity, not convenience.
Life After Ostomy Surgery
While the physical changes are immediate, adapting to life with an ostomy is a gradual process. Most patients go through emotional and practical adjustments before regaining confidence.
Physical Recovery
Initial recovery includes:
- Learning stoma care
- Managing output
- Preventing skin irritation
- Gradually returning to normal activity
With proper education, most patients can independently manage their ostomy within weeks.
Emotional and Psychological Adjustment
It is normal to experience fear, grief, or anxiety after surgery. Body image concerns and lifestyle worries are common, especially early on.
Support systems that help include:
- Ostomy nurses (WOC nurses)
- Peer support groups
- Counseling or therapy
- Educational resources
Over time, many patients report improved quality of life compared to their pre-surgery condition.
Daily Life With an Ostomy
Diet and Nutrition
There is no universal “ostomy diet,” but many people learn which foods work best for them. Key considerations include:
- Staying hydrated
- Introducing foods gradually
- Managing gas and odor through dietary choices
- Chewing food thoroughly
Most individuals return to a varied and enjoyable diet.
Work, Travel, and Exercise
Living with an ostomy does not mean giving up normal activities.
- Most people return to work without limitations
- Travel is fully possible with proper supplies
- Exercise, including swimming and gym workouts, is encouraged after healing
Modern pouching systems are discreet, secure, and designed for active lifestyles.
Intimacy and Relationships
Concerns about intimacy are common but manageable. Honest communication with partners and confidence in pouching systems often resolve initial anxiety. Specialized covers, belts, and accessories can improve comfort and discretion.
Advances in Ostomy Care
Ostomy care has improved dramatically over the years. Today’s products focus on:
- Skin protection
- Secure adhesion
- Odor control
- Comfort and flexibility
- Customization for different body types
Accessories such as barrier rings, seals, and adhesive removers help reduce irritation and improve wear time, making daily management easier and more comfortable.
Breaking the Stigma Around Ostomy
Despite how common ostomies are, stigma and misinformation persist. Many people with ostomies live invisibly among us—working, parenting, traveling, and thriving.
Education plays a crucial role in reducing stigma. Understanding what causes ostomy, why it is necessary, and how manageable life afterward can be helps shift the narrative from fear to empowerment.
Conclusion
An ostomy is not a failure of the body—it is a medical solution that restores health, function, and often life itself. Whether caused by chronic disease, cancer, trauma, or congenital conditions, ostomy surgery enables people to regain control and move forward.
With proper care, modern products, and supportive communities, individuals with ostomies can lead full, confident, and active lives. Knowledge is the first step toward acceptance, and understanding ostomy helps replace uncertainty with clarity and hope.